Designing Self-Powered Breath Sensors to Track Chronic Respiratory Conditions
When it’s resting, the average human body produces about 100 watts of power — energy that could someday power lifesaving medical devices. At the 2022 APS Division of Fluid Dynamics meeting in Indianapolis, Indiana, this past November, Lucy Fitzgerald, a doctoral student in mechanical and aerospace engineering at the University of Virginia, presented new research designing and testing an implantable airflow sensor that harnesses lungs’ own breath for power. Their work was recently published in Royal Society Open Science.
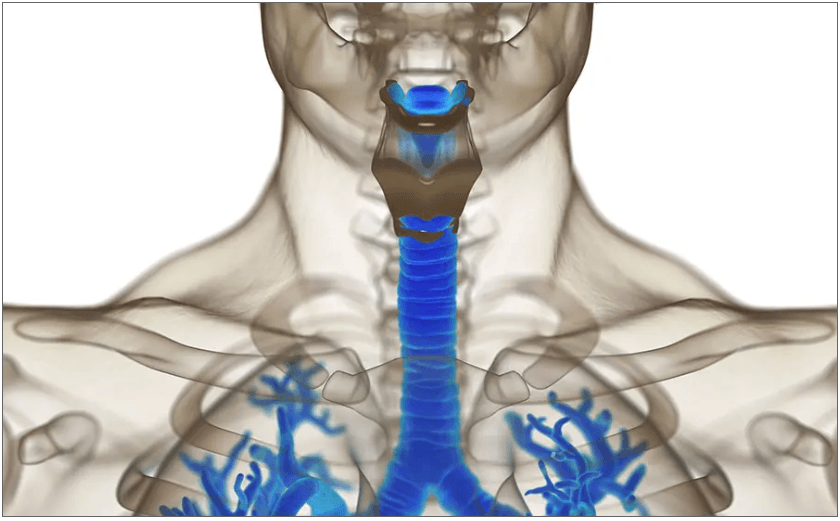
Many patients with respiratory conditions like chronic obstructive pulmonary disease or asthma require, or would benefit from, regular monitoring by a breath sensor. “Most sensing that you see is via a wearable, or something that you breathe into,” Fitzgerald explains. The nasal tubes or chest straps available today are often inconvenient or uncomfortable, and Fitzgerald set out to design a sensor that could be inserted in a person’s airway.
But engineers encounter two major problems when trying to create implantable sensors: “power and real estate,” Fitzgerald says. Stuffing the respiratory system with a bulky sensor burdened by a battery that must be periodically replaced is “really a non-starter. You can’t have a lot of blockage or you’re going to make the problem worse,” explains co-author Daniel Quinn, an assistant professor in engineering at the University of Virginia.
A sensor that harvests energy from what it is sensing — that’s “self-powered by design” — could be well-suited to monitoring airflow in the lungs, the researchers suggest. Engineers have created self-powered-by-design sensors in other contexts — for example, a sensor on a fish’s fin that measures its activity as it swims down a stream. “The flow is both the power source and the thing we’re trying to measure,” Quinn explains.
Fitzgerald and her colleagues set out to “marry these two ideas” and create a sensor that is both implantable and self-powered. They first created a mathematical model of the sensor by combining three sets of equations, predicting how the sensor will move, how it converts mechanical strain to voltage, and how the fluid flow — the breath — will move in and out of the trachea.
Next, the team tested their model on the lab bench. They built the sensor out of a piezoelectric polymer (a material that can generate electric charge when bent) and set up a machine to simulate breath flow. “It’s a big box that’s essentially a programmable lung,” says Fitzgerald.
The simulator could approximate around 200 different “types” of breathing, from sleeping to meditating to jogging, each with different amplitudes and frequencies. The researchers attached a long tube to the simulator, affixed the fingernail-sized sensor to the end of the tube, then attached the sensor to an electrical circuit connected to a computer. Fitzgerald then built software to collect data from both the sensor and the “lung.”
They tested the sensor against many types of breath, comparing its performance to their initial model. They found, for example, that it could distinguish between 28 and 30 breaths per minute.
Some elements of the sensor’s performance surprised the team. “You might just think the faster you breathe, the more power you’re going to generate. But it’s not quite that simple, because the amplitude of your breath changes,” Quinn says. While you can take shallow fast breaths, it’s not really possible to take deep fast breaths, he explains.
“You kind of want an intermediate frequency at a high amplitude that actually gets you the maximum power,” he says — the breathing a person might experience while jogging.
These parameters will depend on the shape and size of the sensor, and will guide the engineers in creating a viable prototype for use in a living system. Their benchtop model, at 12-by-7 millimeters, is too big to go inside an airway, so they are now studying how its functions hold up as it shrinks in size.
Recently, Fitzgerald and Quinn teamed up with a throat surgeon at the University of Virginia to implant a smaller version of their sensor in live, unconscious rabbits. The researchers then used a drug to induce asthmatic breathing in the rabbits, and found the sensor was able to detect signs of the asthma attack in the animals.
In these experiments, the sensor is only in the rabbits’ airways for a few minutes at a time. “Right now, it's more about testing how you would actually install this,” Quinn explains. In the future, the team hopes their work will help lead to a sensor in humans that allows for long-term monitoring.
“Oftentimes, for [chronic respiratory] conditions, you have to have multiple doctor's visits where sometimes they just put a scope down your throat and say, ‘looks good,’” Fitzgerald says. “If you had more continuous monitoring, you might be able to avoid that.”